Research Topics
Health Consequences of a Changing Economy
While the U.S. economy has grown overall, some people are increasingly being left behind. Wages for low-income and middle-class Americans have stagnated, while those for the top have increased. This increasing divergence may be tied to increasing automation, competition from foreign trade, and changes in social and economic policy.
Sociologists like William Julius Wilson and economists like Anne Case and Angus Deaton have posited that fading job opportunities—particularly in manufacturing—have given rise to increases in “deaths of despair” (e.g., suicide and drug overdose). The idea is that a loss of economic opportunities means a loss of hope for the future, unrealized dreams, and – as a result poor health and elevated risk of early death.
In one of our earlier studies, “Economic Mobility and the Mortality Crisis Among US Middle-aged Whites” (2017), we examined how mortality rates among middle-aged white Americans changed over time in counties with low vs. high levels of economic opportunity. We focused on middle-aged white Americans given the alarming growth in mortality rates seen in this group. We found that counties in the bottom 25% of all counties in terms of upward mobility experienced a 5% increase in mortality rates relative to high mobility counties.
Using a natural experiment methodology and data from 1999-2016, we found that deaths from opioid overdose rose dramatically in counties located in areas where automotive plants closed.
We followed this short study up with a more detailed analysis in our “Association Between Automotive Assembly Plant Closures and Opioid Overdose Mortality in the United States” (2020). We started with the hypothesis that job opportunities are critical to a well-functioning economy and public health. We investigated what happened to health outcomes—specifically drug overdose deaths—when long-standing beacons of economic opportunity, automotive assembly plants, closed in the U.S.
Using a natural experiment methodology and data from 1999-2016, we found that deaths from opioid overdose rose dramatically in counties located in areas where automotive plants closed, relative to the same changes in counties where plants did not close. Manufacturing counties with these closures had 8.6 deaths per 100,000 residents more than unaffected counties due to a relative increase in overdose mortality. This effect was particularly larger young, non-Hispanic white men.
Figure 1. Trends in opioid overdose deaths after auto plant closures

Figure 2. Changes in automation and drug overdose mortality across U.S. counties
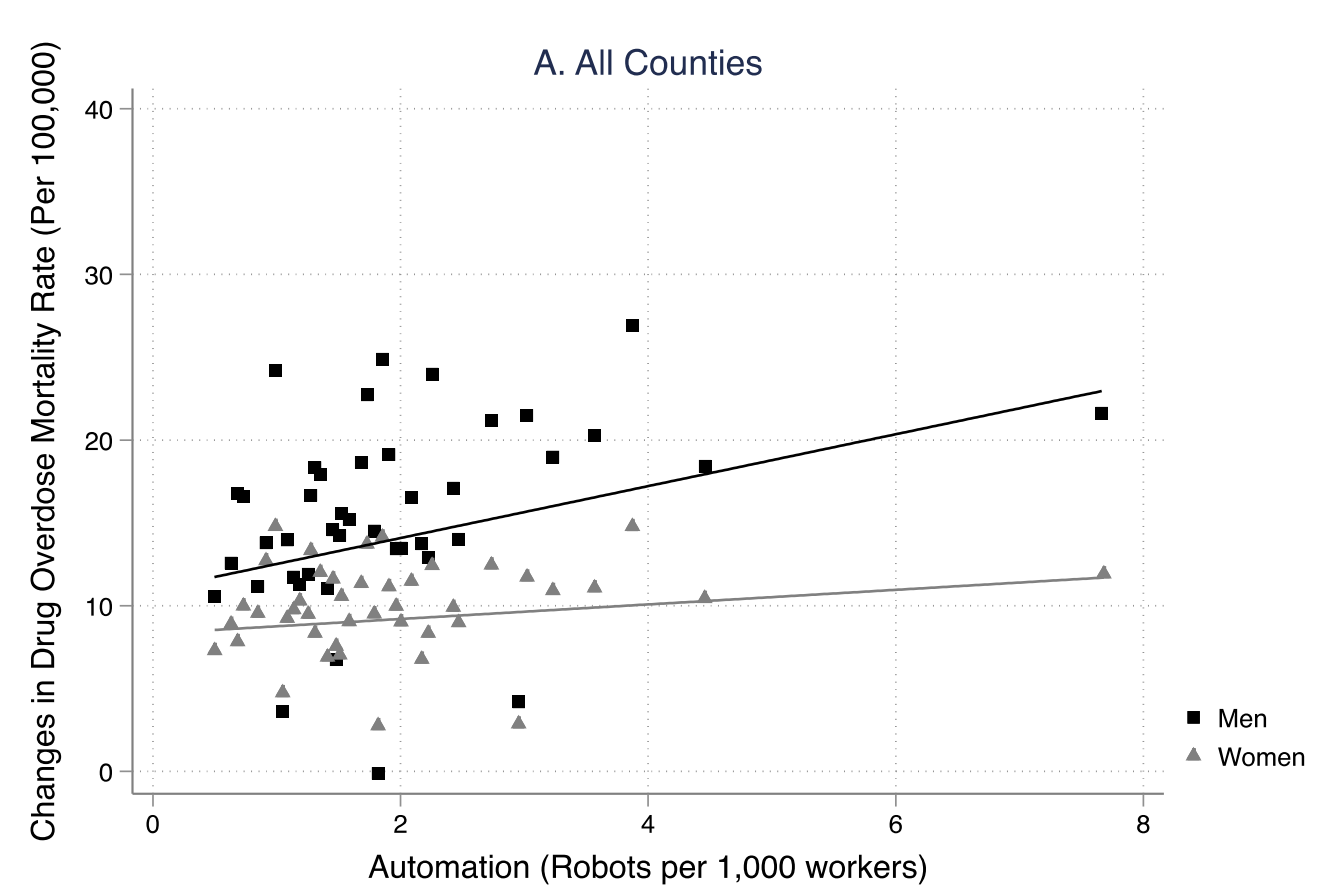
In a report for the U.S. Social Security Administration (SSA), we examined whether automation – a key driver of fading economic opportunities in manufacturing – led to worsening mortality and higher rates of disability claiming in the United States. Using new data on the adoption of industrial robots in U.S. commuting zones, we found that increases in automation can account for 12% of the rise in drug overdose mortality between 1993 and 2007, and 22% and 12% of the rise in Supplemental Security Income (SSI) and Social Security and Disability Insurance (SSDI) applications, respectively, between 2000 and 2007.
We extended this analysis in a 2022 study published in Demography, “Death by Robots? Automation and Working-Age Mortality in the United States.” In this study, we found large effects of automation on overall mortality, drug overdoses, completed suicides, and cardiovascular disease mortality, which varied by age and gender. We also showed in this work how social policies could blunt some of the negative impacts of automation on health.
These findings are consistent with work from other researchers, who have examined the impacts of automation on a range of health and human capital outcomes. They are also consistent with work demonstrating how area-level exposure to foreign trade, which similarly displaces manufacturing jobs, leads to increases in drug overdose deaths.
View Related Research